|
Excerpted from Migraine Brains
and Bodies.
Head and Neck Pain
are common expressions of myofascial dysfunction yet chronic headache sufferers
tend to respond badly to diagnoses of “tension” or
“muscle tension headache.” The labels of
“vascular” headache or “neurological disease” seem more respectable,
more likely to be taken seriously. But “vascular” doesn't stop at
the head; “neurological” isn't restricted to the brain or spine.
Tight muscles and fascia (connective tissue) press, shear, block, and strangle both
blood vessels and nerves throughout the body. Thus “muscle tension
headache” can simply mean a “headache due to tight muscles pulling or pressing
on pain-sensitive structures” but from there it has been a short trip to
“You’re just tense” and “Have you considered psychiatric counseling?” with the clear
implication that...
The pain is not real. YOU are just
crazy.
Many pains do indeed have psychiatric components, but
the psychogenic diagnosis is woefully overdone. (Notice how rarely it is
applied to knee pain, big toe pain, or shoulder pain.) It is
used all too often by the physician, who, when asked for the
underlying cause of head pain, cannot bring himself to say “I don’t
know.” And there's a lot to know. Over 20 muscles (primarily of the
neck) refer (send) pain to the head. Several refer pain specifically to the
eye. At least three refer pain directly to the teeth and jaw for reasons that
will never be relieved by fillings or repeated root canals.
Of particular concern neurologically is strain or compression of the trigeminal nerve
and its branches which mediate tissue inflammation, vasodilation and
vascular permeability in the brain — all issues in migraine. And despite the old belief that muscles
are entirely unrelated to the symptoms commonly diagnosed as migraine, muscles play an important role.
- Botox. for well over a decade (2000), plastic surgeons have verified the muscle-migraine connection
beginning with the observation that Botox injections to muscles of the brow also eliminated migraines.
Why? Because these muscles, when tightened by frowning (and producing the wrinkles which the Botox was intended to block)
were strangling branches of the trigeminal nerve.
Dural Bridge. An extreme example of neuro-muscular interaction, especially likely in persons
with a head-forward posture.
The bridge is connective tissue that connects muscles at the base of the skull (suboccipitals) directly to the dura,
the tough but pain-sensitive tissue surrounding brain and spinal cord. In other words, tight neck muscles can yank
directly on the brain and spinal cord.
Might this cause pain and neurological symptoms? It does. The dura is the outermost layer of the
3-layered meninges and one of the symptoms of meningitis is a horrific headache (and nausea and sensitivity to light).
Although recognized for at least 20 years (1995), imaged in MRI, dissected and plasticized, it does not yet appear
in standard medical textbooks (or migraine books). It is rarely considered in migraine diagnosis, no matter how severe
the pain or poor the posture may be.
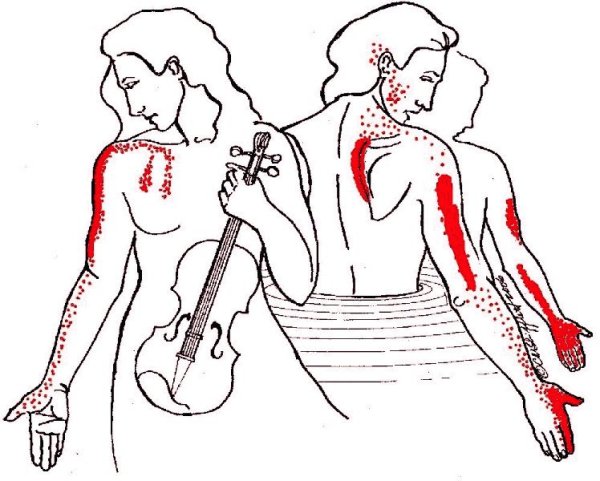
Thoracic Outlet Syndrome. This painful condition, strongly linked to scalene and subclavius muscles of neck and shoulder
can underlie chronic migraine, especially if accompanied by
the symptoms of Carpal Tunnel Syndrome (pain or tingling in the thumb and first 2 fingers). Many cases of carpal tunnel
problems and chronic intractable migraine may actually be coming from the shoulder, in a terrible combination of
dysfunctional or inflamed muscles, compressed nerves, and blocked blood circulation.
If irritated muscles and nerves fire off
an inflammatory response and vasodilation, is the resulting headache
muscular, neurological, or vascular? The answer may be
“all of the above” because amazingly enough, it all
functions together — or dysfunctions together. It may seem odd, but it's just basic physiology.
For patient
or physician, the following pain patterns may look surprisingly
familiar and will, we hope, point the user in the direction of truly
effective treatment.
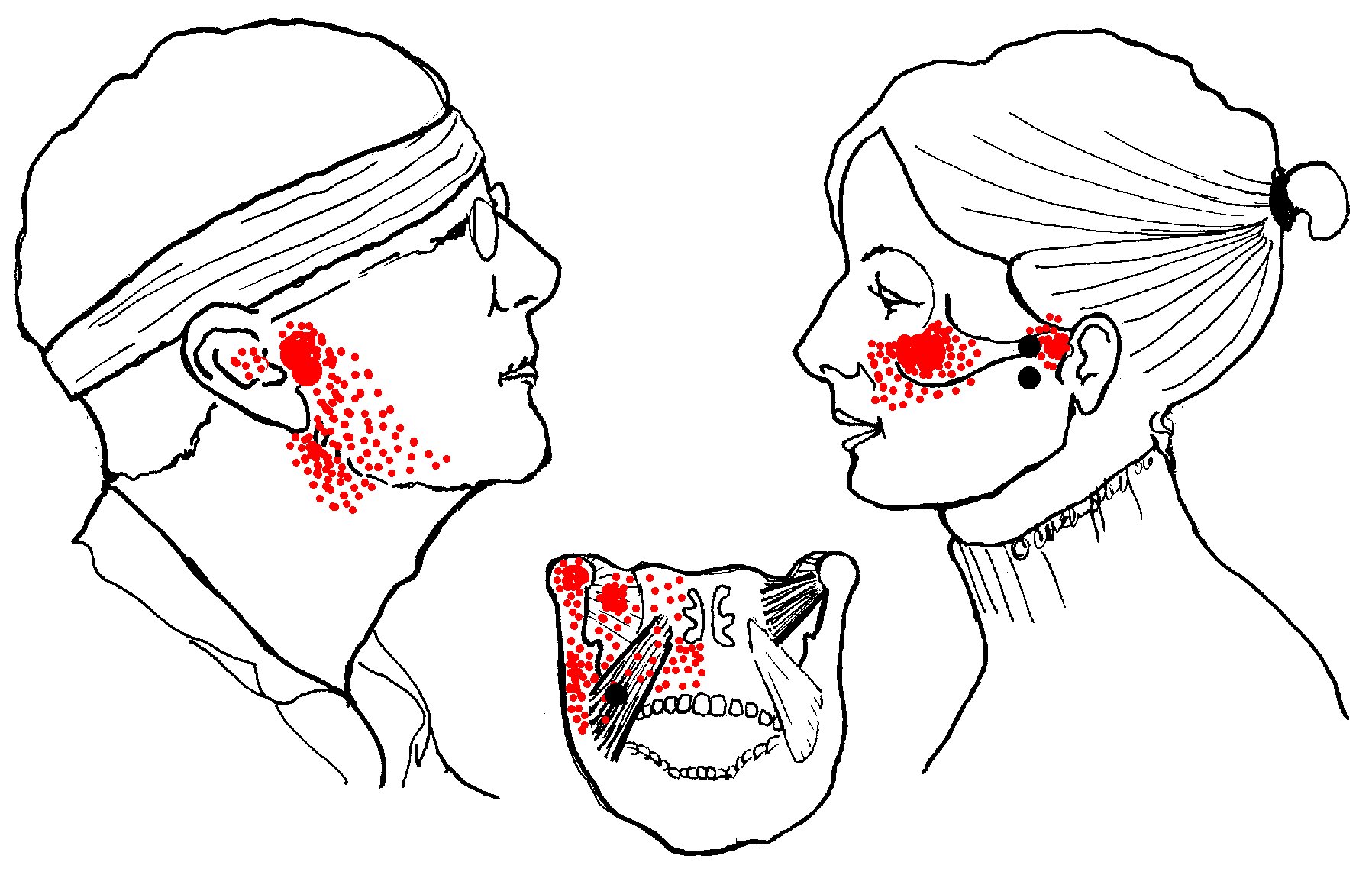
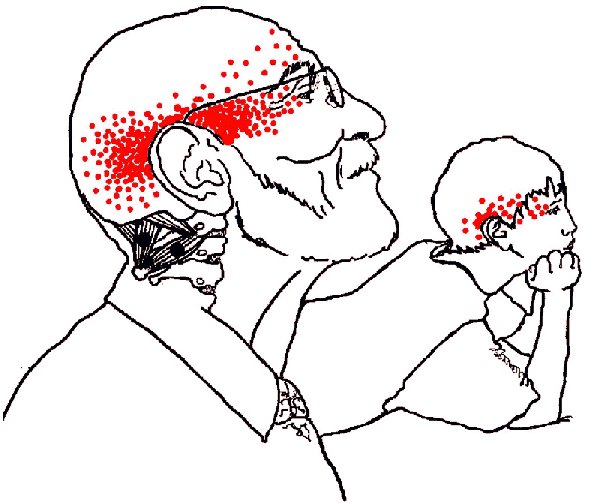
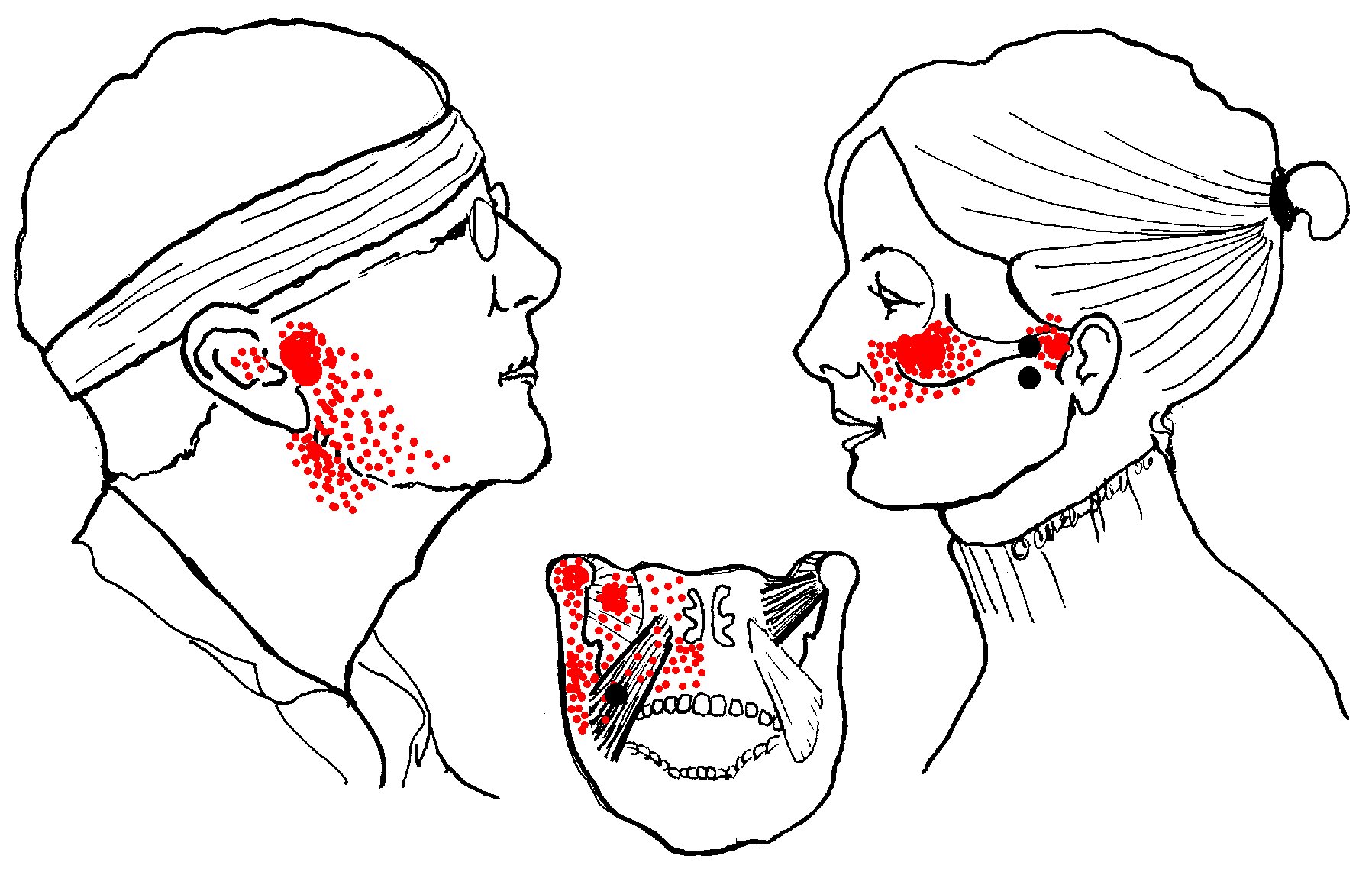
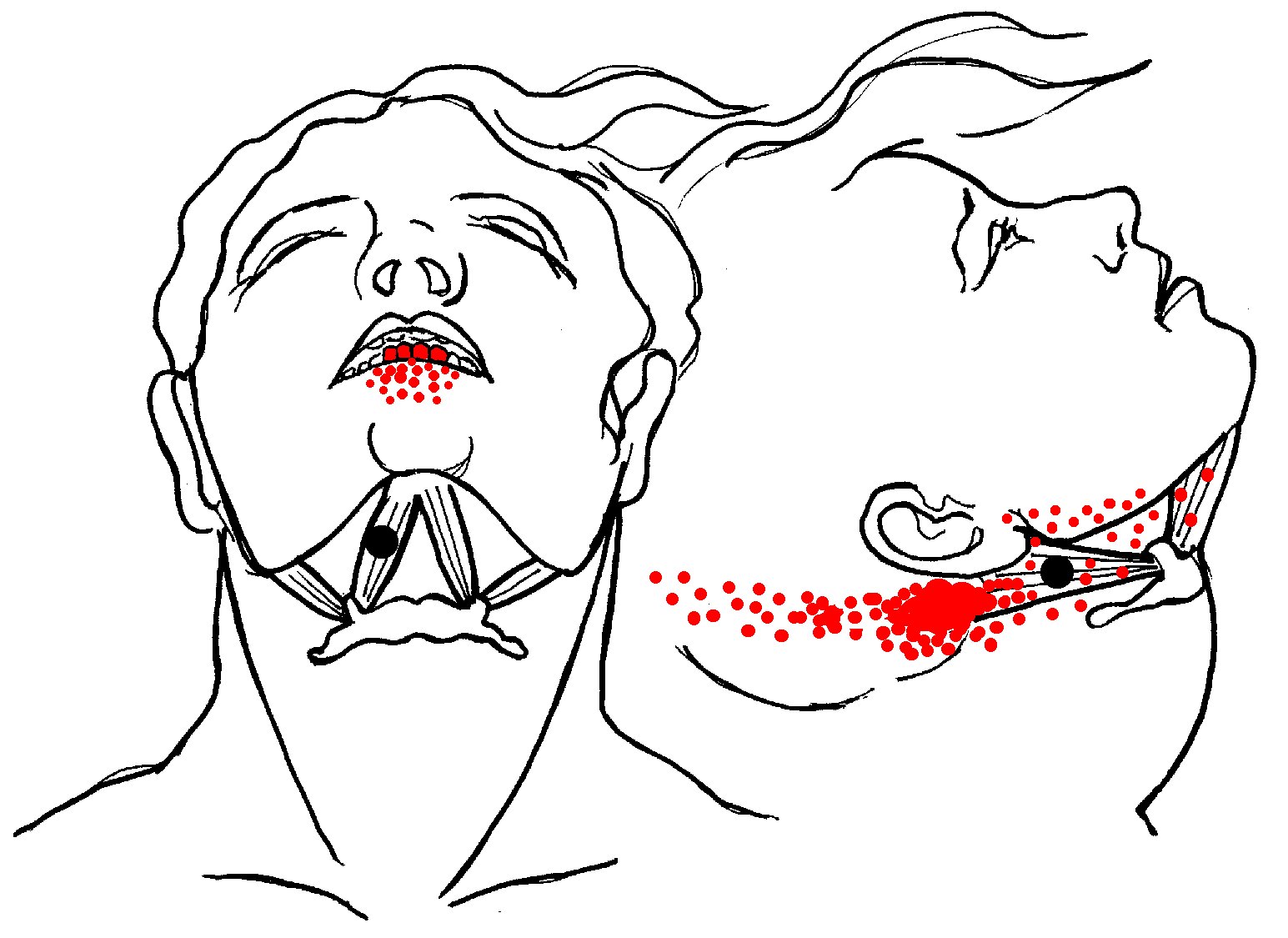
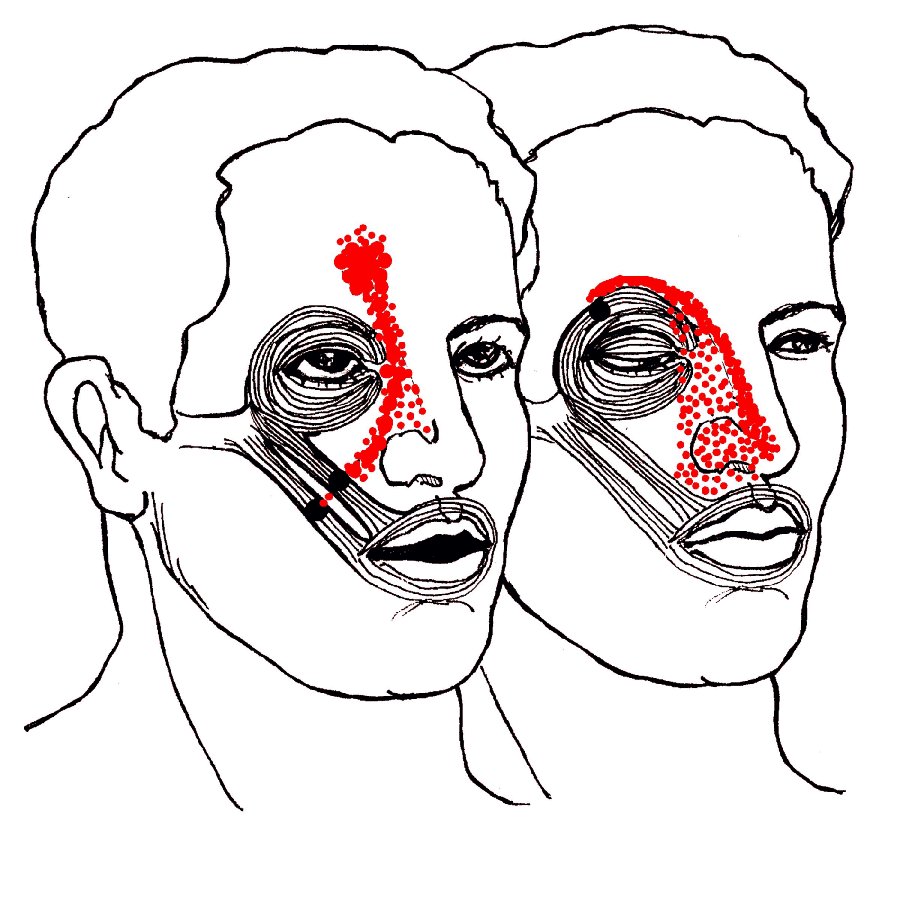
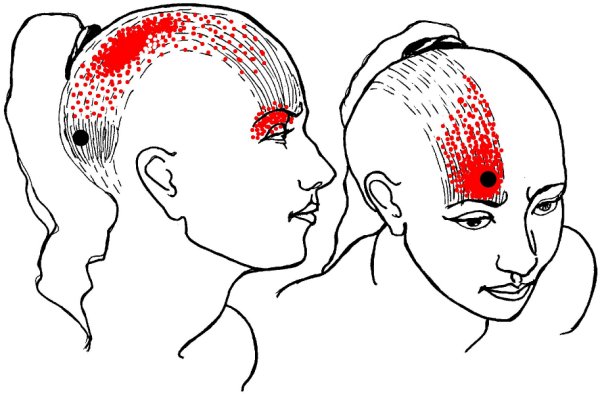
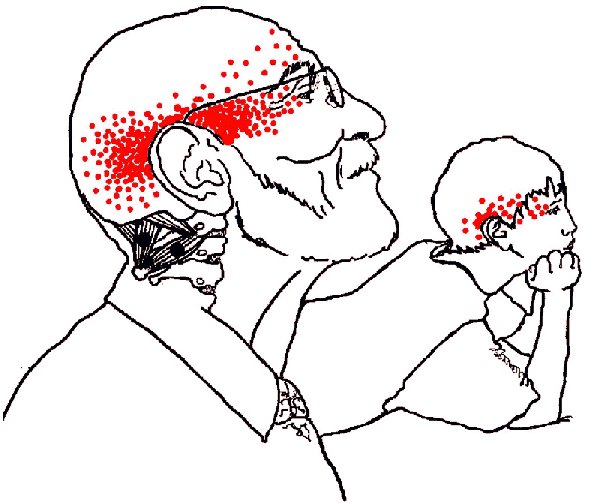
In the following
illustrations, black dots indicate common trigger point locations;
red areas indicate the pain referred by the trigger point. You can
evaluate these muscles with the Cervical and Masticatory Tests
excerpted and adapted from our
Range-of-Motion
Testing Charts. That is, your ability to touch your chin to your chest (or not) may be a huge clue to the
mystery of your migraines.
- Upper Trapezius > Tension headache and “bursitis.” The
trapezius muscle of the back and neck is the single muscle most
likely to have trigger points in both adults and children.
Upper trapezius refers a "fish-hook" pain pattern up the back
side of the neck to the head, and around the temple to the eye.
There may be goosebumps to upper arm and thigh possibly with nausea
and visual disturbances including nausea and light sensitivity. Problems often begin with heavy bags or
purses, balancing phones between head and shoulder,
or imbalances and strain by tight SCM or scalene muscles.
The nauseating pain of a one-sided
trapezius headache is commonly diagnosed as migraine.
(Additional diagnoses of bursitis and back pain may arise from the upper and
lower fibers of the same muscle;
see Introduction to Shoulder Pain) and the muscles behind "frozen shoulder."
Trapezius and the sternocleidomastoid muscle (SCM, below) both produce a wide range of
neurological symptoms because both muscles are supplied by the spinal accessory nerve,
a cranial nerve (CN IX). That is, the nerve that runs these two postural muscles travels directly
from and then reports directly back to the brain.
But there's more. The vagus nerve (another cranial nerve, CN X, responsible for many autonomic
symptoms) blends its fibers with the accessory nerve. Thus poor posture alone (especially
a head-forward position) can trigger common symptoms of migraine which do not respond to migraine medications.
- Sternocleidomastoid (SCM)
 > Dizziness, nausea, “migraine” and “sinus” pain.
Because of its intimate involvement with brain stem and
the vagus nerve, the SCM muscle of the neck produces a long
list of neurological and pain symptoms. These appear primarily in
the head and face but may also present
as nausea, motion sickness, and balance problems.
> Dizziness, nausea, “migraine” and “sinus” pain.
Because of its intimate involvement with brain stem and
the vagus nerve, the SCM muscle of the neck produces a long
list of neurological and pain symptoms. These appear primarily in
the head and face but may also present
as nausea, motion sickness, and balance problems.
Symptoms are commonly mistaken for migraine,
sinus infections, inner-ear problems, trigeminal
neuralgia and so on.
Although SCM has one of the most extensive
patterns of pain and dysfunction, it is one of the easiest muscles to
self-treat.
-
Scalenes > “Thoracic outlet” and “carpal tunnel”
syndromes; chest, arm, and upper back pain.
Scalenes contribute to severe tension headache and are
one of the leading causes of “carpal tunnel syndrome.” On the list
of a half-dozen possible causes, the carpal tunnel itself is
dead last, one reason why carpal tunnel surgery
is so often ineffective. Check before you cut!
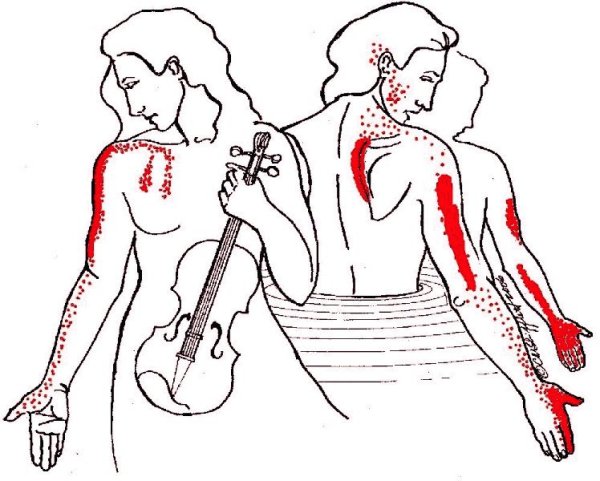
Notice also the fingerlike projections of pain extending down the chest.
This is easily confused with angina. If you think you are having
heart problems, see a doctor immediately!
If, however, no cardiac problems are found, consider
other muscles, especially if the chest pain was accompanied by
a tingly thumb or index finger. Scalene pain typically extends down
the upper arm, skipping the elbow. There may also be severe pain
at the vertebral border of the scapula.
All of these patterns may be painfully familiar to wrestlers and
Aikidoists who have suffered too many “neck-a-nages.”
In Aikido, students who don't understand kokyu-nage techniques
(they are based on balance and timing) tend to interpret what they think they see
as: “Swing your partner around by the neck then drop him on
his head.” It is a painful variation on the game of “Hangman.”
In professional football, doing the same
thing to a large, padded, extremely fit refrigerator-sized
opponent by grabbing his face-guard will get you an instant
15-yard penalty, for very good reason.
The consequences of this action can be hideously
painful and / or disabling. The electrical supply for arm and fingers (the brachial plexus, a network of nerves)
originates in the neck. One of these, the median nerve, supplies the thumb, index, and half
the middle finger. It also passes under the carpal tunnel of the wrist.
If pain and tingling in thumb and index fingers is diagnosed as entrapment
of the median nerve, the patient may be referred for carpal tunnel surgery. (Note that pain in the
ring and pinkie fingers has nothing to do with the median nerve.) If the problem
is identified as scalene entrapment of the brachial plexus,
the current treatment is surgical removal (“scalenectomy”)
of the anterior scalene m and the first rib
Unfortunately, this surgery can cause more problems than it cures.
Scalene problems are better treated by relaxing the involved muscles and their trigger points, and by
pressing the first rib back into its proper position.
- Masseter >
TMJ, tinnitus, “sinus”, and toothache. For
its size and weight, the masseter is the strongest muscle in the
body and its effects are for from small.
 It refers
pain to both upper and lower molar teeth, causes TMJ dysfunction,
earache and pain over the eyebrow. It refers
pain to both upper and lower molar teeth, causes TMJ dysfunction,
earache and pain over the eyebrow.
Prozac and related anti-depressants such
as Paxil specifically cause tightness in this muscle.
If you're grinding your teeth at night and waking with
a headache, ask your doctor about taking the medication during the daytime
when you can be more aware of clenching and tooth-grinding which
tense the masseter but also strain the temporalis . . .
- Temporalis >
"Tension / sinus" headache, TMJ and
toothache in upper teeth.
 Combine a
head-forward position with a pipe and long hours of playing
the violin (see the scalene pain pattern, above) and what do you
get? Combine a
head-forward position with a pipe and long hours of playing
the violin (see the scalene pain pattern, above) and what do you
get?
“Elementary!” cries Dr. Watson. “Head
pain, tooth pain, and extreme tooth sensitivity to heat/cold and
vibration.”
You may wisely eschew “The Seven Percent Solution*” in favor of
directions to massage the temples to relieve tension headaches.
But to make it more effective, notice the
location of the trigger points and their specific areas of pain.
Temporalis is remarkable for spoke-like lines of pain up into the
temple and down into the upper teeth. Follow these lines and you
will feel distinct taut bands. Massaging them may provide temporary relief.
But the best approach is to follow the taut bands down to their
trigger points (feel for small lumps) located as shown near the cheekbones
and adjacent to the ears.
*Opioids risk addiction and rebound headaches.
- Pterygoids> TMJ and “sinus” pain. These muscles
are the secret of success in alligator wrestling. These jaw-opening muscles are extremely weak compared to the
powerful jaw-closing masseter and temporalis. They can be strained by such simple things as eating sticky, chewy foods.
The lateral pterygoids (at right) help to open the jaw and push it forward.
They commonly develop trigger points that cause laterial deviation
on opening the jaw, in turn causing pain and/or clicking in the TMJ joint. They can block
drainage from the maxillary sinus causing still more pain. They
are also linked to tinnitis and can entrap the buccal nerve (a branch of the trigeminal nerve) causing numbness
/ tingling in the cheek (see buccinator, below).
In combination with the masseter muscles, medial pterygoids support the jaw like a sling.
Masseter is on the outside, medial pterygoid inside. They work together
(to pull the jaw up and closed) but produce different pain patterns. Medial pterygoid refers diffuse pain
to the mouth involving the floor of the nose, tongue, throat and
hard palate. There may be pain below and behind the TMJ joint, pain and/or
stuffiness of the ear, difficulty swallowing, lateral deviation
and possibly pain on opening the jaw.
Medial pterygoid muscle can also entrap the lingual nerve (yet another branch of the trigeminal) producing the odd symptom of a bitter,
metallic taste in the mouth (which the patient may not connect with
other symptoms and may not report for fear of being thought “crazy.”)
- Buccinator > Cheek pain. Buccinator forms the wall of cheek and mouth. It's
 the part that puffs out when playing the trumpet (for which it is named), blowing up balloons
or stuffing the mouth too full. Pain may also appear suddenly following dental/orthotic work.
the part that puffs out when playing the trumpet (for which it is named), blowing up balloons
or stuffing the mouth too full. Pain may also appear suddenly following dental/orthotic work.
There are no entrapments by the muscle
itself, but the lateral pterygoid can entrap the buccal nerve
which supplies the skin and mucous membrane, causing numbness in this area. The
muscle can cause local pain deep in the cheek while
chewing, commonly misdiagnosed as TMJ dysfunction.
- Digastric > Neck pain and and toothache in the lower
incisors. Digastric ("two bellies") assists the lateral pterygoid in opening
the jaw against the counterforce of the far more powerful
temporalis and masseter muscles. The upper portion can entrap the
external carotid artery and auricular artery decreasing blood flow
to the brain.
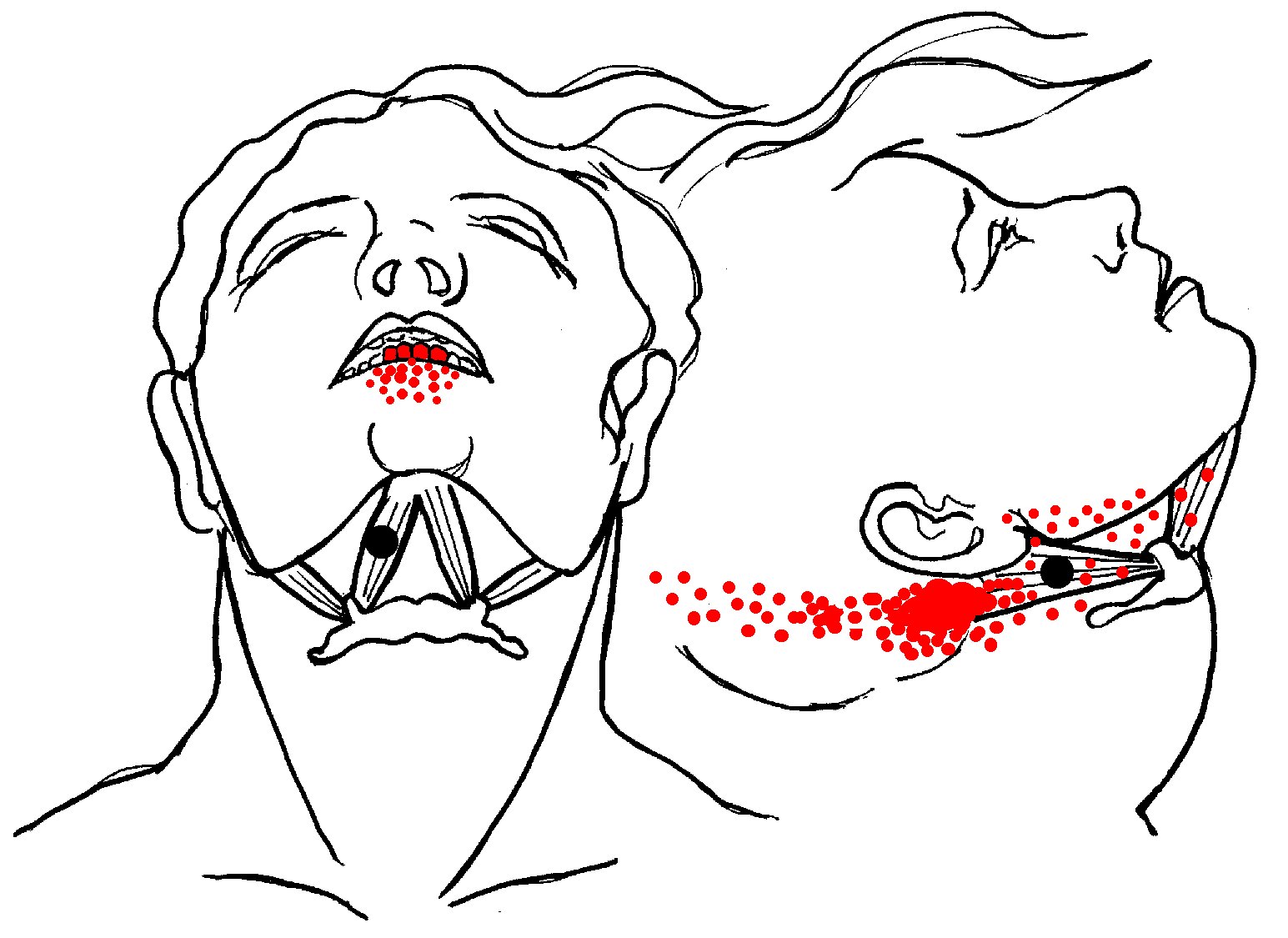 It is strained by retrusion (pulling back) of the jaw (as in playing
the clarinet) or by holding a violin in place by gripping it with the chin.
Like other neck muscles, it is commonly damaged in whiplash injuries.
.
It is strained by retrusion (pulling back) of the jaw (as in playing
the clarinet) or by holding a violin in place by gripping it with the chin.
Like other neck muscles, it is commonly damaged in whiplash injuries.
.
Trigger points in the front (anterior) section of the muscle send pain to the four lower incisor teeth and the
alveolar ridge. There may also be pain in the tongue, a feeling of a
persistent lump in the throat and difficulty swallowing.
Trigger points in the back (posterior) section, refer pain to the upper sternocleidomastoid (SCM) muscle,
with pain to the throat felt as far back as the rear of the head (occiput).
The lump in the throat is the hyoid bone, to which digastric attaches.
This bone must rise to allow swallowing, but cannot when the muscle fails to control it properly.
- Orbicularis > Nose and cheek pain (shown with
zygomaticus, below right). A trigger point in orbicularis refers pain
along the eybrow, alongside the nose to the upper lip. There may
be visual disturbances and problems with jumpy print in reading,
along with droopy eyelid (ptosis).
- Zygomaticus
> Nose, cheek, and forehead pain (shown with orbicularis, below left).
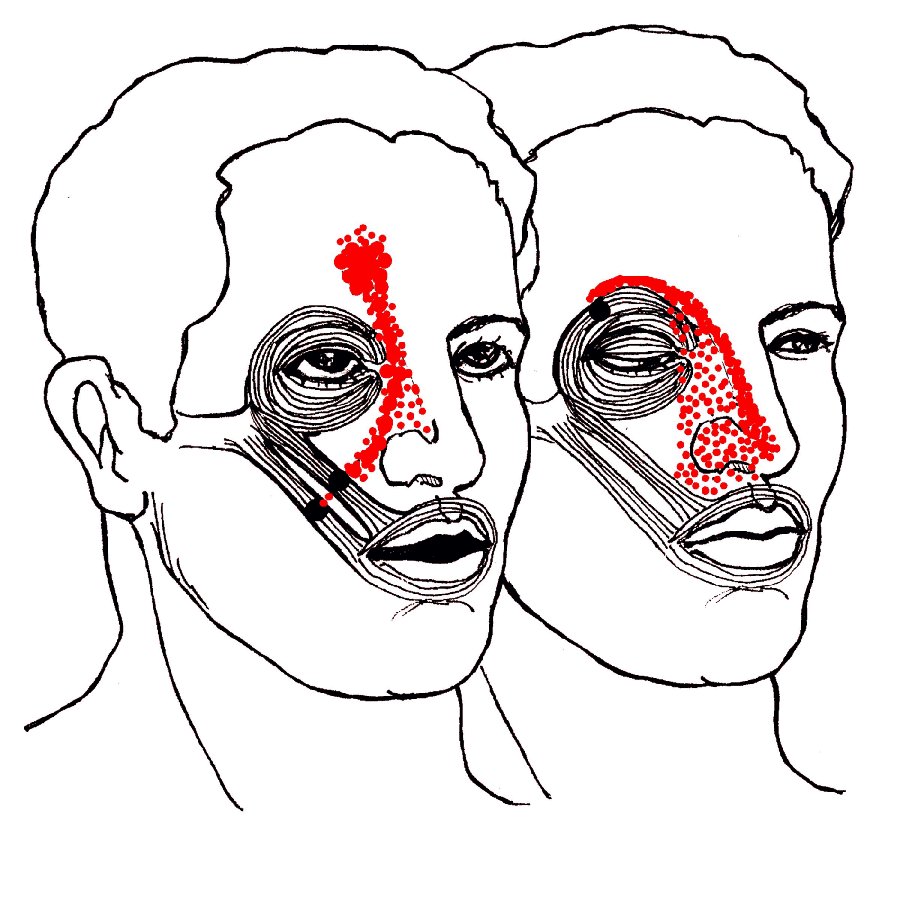
Orbicularis and zygomaticus are the only two muscles that refer pain to
the nose. Both patterns are commonly mistaken for sinus infection but may
be due to a blow to the eye or simply smiling too long at the reception.
Zygomaticus can entrap blood vessels that travel from
cheek to nose and up to the forehead.
The resulting pain is not “sinus,” it is a muscle cramp due to
reduced blood and oxygen supply — but no less painful.
- Occipitofrontalis > Temporal and eye pain.
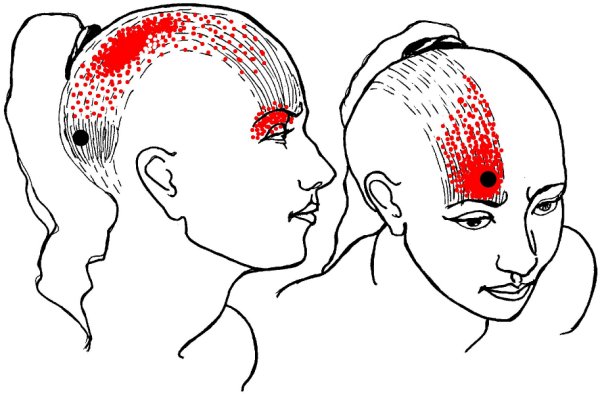
Trauma to the
scalp fascia or the occipitalis at the back of the skull can
transmit pain through the head and into the eye. Trauma may
include a blow to the back of the head, strain from a tight
ponytail or bun, or the weight of long, heavy hair.
When a man struck the top of his head on the corner of
a cabinet, the result was a slight puncture wound in the scalp but a brutal
pain in the eye that lasted for days.
Frontalis helps open the eyes, raises the
eyebrows, and wrinkles the forehead into “worry lines.”
It is commonly used by biofeedback practitioners to monitor muscle tension.
Trauma to frontalis (whether a blow to the forehead or habitual
frowning) can cause severe frontal headache often diagnosed
as migraine. Frontalis is one of the muscles that definitively proved
the muscle-migraine connection.
Botox injections paralyzed the
frontalis, eliminating worry lines but they also had the
surprising side effect of halting chronic migraines. Or maybe
not so surprising, as frontalis entraps the supraorbital nerve.
The related corrugator supercilii (at the top of the nose between
the eyebrows) compresses branches of the supraorbital nerve along
with the supratrochlear nerve and branches of the supraorbital
nerve. All of these are branches of the trigeminal nerve which is
heavily involved in migraine. You can treat trigger points with
great results — or, avoid compressing those muscles in the first place.
Your frown may be giving you a headache!
- Splenius Capitis > Occipital neuralgia and “word processor headache”.
Splenius cervicis (below, left) and splenius capitis are almost always injured in auto
accidents, regardless of the direction of
the blow. They are also strained in head rolling movements in
exercise classes, chronically injured by head forward postures and by
computer use or other reasons for sitting with head held
forward and turned to the side. Splenius capitis (shown below, right)
typically causes a pain at the top lateral side of
head. It is similar to that produced by SCM, but shifted slightly to the side.
- Splenius Cervicis > Neck pain, eye pain, and blurred
vision. Splenius cervicis (above, left) is strained in the same ways as splenius
capitis (above, right) but the results are even more painful. A trigger point
high in the neck portion of the muscle sends pain through
the head from the occiput and into the eye. Even without the pain, there
may be blurred vision. The lower trigger point refers pain to
the angle of the neck. Reading under a drafty air conditioner or
riding a bicycle or motorcycle with head forward with a cold wind whipping
around the edge of the helmet is damaging to these muscles.
- Semispinalis Capitis > Head pain and occipital
neuralgia. This muscle of spine and neck is heavily involved in tension and
cervicogenic headache. It is commonly injured in whiplash and auto accidents. You can injure it more slowly but just as
effectively with a chronic head-forward position. Migraine pain that begins in the back of the head, may begin here.
When
strained, semispinalis can entrap the greater occipital nerve which in turn causes numbness, tingling
and/or burning pain extending over the back of the head to
the top (vertex) of the head.
It may be difficult or painful to touch chin to chest, and sufferers may be unable to
bear the pain of laying the back of the head on a pillow.
Relieve nerve pain with cold.
Relieve muscle pain with moist heat.
In either case, look for the origin of the pain which is rarely the spot where it hurts.
- Semispinalis Cervicis [not shown] > Even more head pain.
This muscle typically
produces a vague band of pain from occiput along side of head to
just behind orbit (similar to suboccipital pain pattern).
- Longus Capitis, Longus Colli [not shown]> Neck, ear, and eye pain.
A pain in the neck, and surprisingly, pain in the eye and ear and
possibly the forehead (more “sinus” pain!) as well. Almost always injured
in whiplash. It may even calcify.
- Multifidi and Rotatores [not shown]> Basal skull pain, neck pain
and scapular pain.
This pain arises from the tiny muscles that
run between the individual vertebrae of the spine.
- Levator scapula [not shown]> The Number One cause of "wry" or "stiff neck"
and the second most common shoulder girdle muscle to have trigger points. (Trapezius is Number One.)
Working with
trapezius, levator shrugs the shoulders and helps prevent forward
flexion of the neck, hence it is also damaged in whiplash
injuries. In daily life, it is strained when shoulders
are chronically hunched, either in stress,
or through attempting to keep a strap from sliding off the
shoulder, especially when the muscle is cold or fatigued.
Pain in the angle of the neck and along the vertebral border
of the scapula may be so severe that patient cannot move the neck at all.
- Suboccipitals > Temporal and eye pain.
 The four pairs of
suboccipital muscles cause deep aching pain running in a
band from the back of the head to the orbit of the
eye, possibly with balance problems and dizziness.
The four pairs of
suboccipital muscles cause deep aching pain running in a
band from the back of the head to the orbit of the
eye, possibly with balance problems and dizziness.
At least one of these (the rectus capitis superior
minor) attaches directly to the dura mater of the spinal cord.
When traumatized it can produce odd visual and neurological
symptoms to the point of seizures.
Suboccipitals cause problems in persons in children who watch TV lying with
chin propped on hands. They may be strained or hypertrophied ("overgrown") in anyone who habitually holds the head
in position with chin up and neck flexed backward, a necessity in head-forward posture and common
in those who wear bifocals.
- Omohyoid [not shown] > Head, neck, shoulder, and back pain. This small muscle
(actually missing from many anatomy books) can cause disabling pain and
dysfunction. It's just one of the several muscles that attaches to
the hyoid bone. The other end attaches to the scapula
at the back of the shoulder. Aside from the severe pain in shoulder,
neck, and jaw (which often appears after a bout of coughing or
vomiting) there may also be weakness and tingling down arm and fingers
and symptoms of thoracic outlet syndrome. Pain patterns may be confused with
that of the scalenes or levator scapula.
- Soleus >
Heel and calf pain, sacral pain and cheek (facial) pain.
One of the outstanding examples of long-distance
pain referral from muscles. This muscle of the calf sends
pain to the calf and heel (commonly known "jogger's heel") — but there's more.
 Pain from this muscle also appears in the
sacrum at the sacro-iliac joint and then reappears in the face and
jaw where it may fire off trigger tooth pain, symptoms of TMJ and migraine.
Pain from this muscle also appears in the
sacrum at the sacro-iliac joint and then reappears in the face and
jaw where it may fire off trigger tooth pain, symptoms of TMJ and migraine.
“But,” you say, “migraine is vascular!”
Indeed it is — and the soleus is the
other end of the cardio-vascular system. It is known as “The Second
Heart” because its pumping action returns blood from the
lower extremities to the heart. If feet are cold, it is possible to stop many full-blown
migraines by working adductor and calf muscles.
“But,” you say, “migraine is neurological!”
Indeed it is — and tightness and restriction
can cause serious impingement on
neurovascular structures including the femoral artery and femoral vein,
entrapped when passing through the adductor hiatus of the adductor magnus.
The soleus can entrap the posterior tibial nerve, vein, and artery. A slip of soleus (plantaris),
can also entrap the popliteal
artery at the back of the knee.) Impact can be so severe that
the patient may lose deep tendon reflexes. With all that, it is no
surprise that a sufferer might have cold feet, and that blood might tend to stay
in the head. (Flight suits and medical anti-shock trousers (MAST) have the same effect.
These are essentially blood pressure cuffs for the legs and lower body. They prevent shock by
keeping blood in the head and torso and they do it so well that their use is contra-indicated for bleeding head and chest wounds.)
Symptoms can result from failure to stretch out after using the thigh machines
at the gym or engaging in the adductor-intensive “runway walk.”
More problems can arise from footwear. Whether you call them “pumps” or “cowboy boots”)
high heel shoes can cause jaw and head pain. It may be hard to believe, but it is often true.
Knee-high stockings with tight, constricting bands will also do the job. Consider also a soldier who never had a headache in his life until
he caught shrapnel in the calf.
When the soleus can no longer function as a second heart, there can be side
effects far worse than migraine. Pooling and subsequent
clotting of blood in the lower legs becomes deep
vein thrombosis (DVT). It is also known as “airline thrombosis” named for the
consequences of hours of inactivity in cramped quarters.
The condition is very real, but sadly mis-named. It is far more common from long hours of sitting at a
desk or on a couch than from (comparatively rare) airline travel.
|
 > Dizziness, nausea, “migraine” and “sinus” pain.
Because of its intimate involvement with brain stem and
the vagus nerve, the SCM muscle of the neck produces a long
list of neurological and pain symptoms. These appear primarily in
the head and face but may also present
as nausea, motion sickness, and balance problems.
> Dizziness, nausea, “migraine” and “sinus” pain.
Because of its intimate involvement with brain stem and
the vagus nerve, the SCM muscle of the neck produces a long
list of neurological and pain symptoms. These appear primarily in
the head and face but may also present
as nausea, motion sickness, and balance problems.
 It refers
pain to both upper and lower molar teeth, causes TMJ dysfunction,
earache and pain over the eyebrow.
It refers
pain to both upper and lower molar teeth, causes TMJ dysfunction,
earache and pain over the eyebrow.
 Combine a
head-forward position with a pipe and long hours of playing
the violin (see the scalene pain pattern, above) and what do you
get?
Combine a
head-forward position with a pipe and long hours of playing
the violin (see the scalene pain pattern, above) and what do you
get?
 the part that puffs out when playing the trumpet (for which it is named), blowing up balloons
or stuffing the mouth too full. Pain may also appear suddenly following dental/orthotic work.
the part that puffs out when playing the trumpet (for which it is named), blowing up balloons
or stuffing the mouth too full. Pain may also appear suddenly following dental/orthotic work.
 It is strained by retrusion (pulling back) of the jaw (as in playing
the clarinet) or by holding a violin in place by gripping it with the chin.
Like other neck muscles, it is commonly damaged in whiplash injuries.
.
It is strained by retrusion (pulling back) of the jaw (as in playing
the clarinet) or by holding a violin in place by gripping it with the chin.
Like other neck muscles, it is commonly damaged in whiplash injuries.
.
 The four pairs of
suboccipital muscles cause deep aching pain running in a
band from the back of the head to the orbit of the
eye, possibly with balance problems and dizziness.
The four pairs of
suboccipital muscles cause deep aching pain running in a
band from the back of the head to the orbit of the
eye, possibly with balance problems and dizziness.
 Pain from this muscle also appears in the
sacrum at the sacro-iliac joint and then reappears in the face and
jaw where it may fire off trigger tooth pain, symptoms of TMJ and migraine.
Pain from this muscle also appears in the
sacrum at the sacro-iliac joint and then reappears in the face and
jaw where it may fire off trigger tooth pain, symptoms of TMJ and migraine.